Contents
- Understanding Infant Feeding Basics: Why Frequency Matters
- Developmental Readiness: When to Expect Longer Intervals
- Breastfed Babies and the 4-Hour Mark
- Formula-Fed Babies: A More Predictable Journey to 4 Hours
- Key Signs Your Baby is Ready for a 4-Hour Feeding Schedule
- Transitioning to a 4-Hour Schedule: Practical Steps
- Important Feeding Guidelines for Babies (Under 1 Year)
- Introducing Solids: How it Impacts Feeding Schedules
- Addressing Common Challenges: Colic, Overtiredness, and Cluster Feeding
- Infant Colic and Feeding Frequency
- Cluster Feeding
- Overfeeding and Weight Gain Concerns
- Night Feedings and Sleep Disruptions
- The Role of Parental Intuition and Professional Guidance
Navigating infant feeding can be one of the most consuming aspects of new parenthood, often leading to a myriad of questions and concerns. A common milestone many parents anticipate is when their baby can consistently go longer stretches between meals, particularly the eagerly awaited when can babies go 4 hours between feedings. Understanding this transition involves more than just a clock; it’s deeply rooted in a baby’s developmental milestones, feeding method, and individual cues. This guide will explore the factors influencing feeding intervals, offering practical advice and expert insights to help parents determine the optimal time for this significant shift, ensuring both adequate nutrition and improved rest for the entire family. Effective baby feeding schedule management hinges on recognizing hunger cues and adapting to a baby’s unique developmental needs, whether they are breastfeeding or formula feeding.
Understanding Infant Feeding Basics: Why Frequency Matters
The journey of infant feeding begins with understanding a newborn’s unique physiological makeup. On day one of life, a baby’s stomach is incredibly tiny, roughly the size of a marble, capable of holding only 1 to 1.4 teaspoons of liquid. This limited stomach capacity is the primary reason why newborns require very frequent feedings, often every 2 to 3 hours, regardless of whether they are breastfed or bottle-fed. As the baby grows, their stomach stretches and matures, allowing them to consume larger volumes of milk or formula at each feeding.The digestive system maturity also plays a crucial role in feeding frequency. Breast milk, being perfectly tailored for infants, is easily digested and empties from the stomach much quicker than formula. This inherent difference means breastfed babies generally feed more frequently than their formula-fed counterparts. Both types of feeding, however, emphasize “on-demand” feeding in the early weeks. This approach ensures the baby receives adequate nutrition for rapid growth and weight gain, laying a strong foundation for future feeding patterns. Parents are encouraged to observe their baby’s hunger cues rather than strictly adhering to a rigid schedule during this initial phase.
Developmental Readiness: When to Expect Longer Intervals
The ability for a baby to go 4 hours between feedings is a significant developmental milestone, generally linked to several factors including age, weight, and overall physiological maturity. The American Academy of Pediatrics (AAP) provides general guidelines, but individual variation is key. Typically, this extended interval becomes feasible as a baby approaches 2 to 4 months of age, when their baby’s weight gain is robust, and their stomach can comfortably hold more milk or formula.
Crucial developmental milestones also support this progression. For instance, improved head control, which usually develops around 4 to 6 months, is an indicator of increased physical strength and readiness for longer periods of activity between feeds, and eventually, for the introduction of solid foods. Babies also become more efficient at feeding as they grow, meaning they can consume a sufficient amount in a shorter time, allowing for longer intervals before hunger returns. Observing consistent feeding patterns and a baby’s overall health and energy levels provides invaluable insight into their readiness for such changes.
Breastfed Babies and the 4-Hour Mark
Breastfeeding patterns are inherently more dynamic than bottle feeding due to the rapid digestion of breast milk and the intricate supply-and-demand mechanism of lactation. In the first few weeks, La Leche League International recommends 8 to 12 feedings daily, emphasizing the importance of not letting a newborn go more than 4 hours without feeding, even if it means waking them. This frequent nursing establishes the mother’s milk supply and ensures appropriate newborn feeding and weight gain.
As a baby matures and breastfeeding becomes well-established, typically around 1 to 3 months, the frequency naturally begins to decrease. Your baby may start taking in more milk in less time at each feeding, leading to longer stretches.
- 1 to 3 months: Feedings usually occur 7 to 9 times within a 24-hour period.
- 3 months: The frequency often reduces to 6 to 8 times a day.
- 6 months: Babies tend to feed around 6 times daily.
- 12 months: Nursing may decrease to about 4 times a day, with solid foods providing additional nutritional needs.
It is common for breastfed babies to engage in “cluster feeding,” where they feed more frequently during certain periods (e.g., late afternoon and evening) and less at others. This can sometimes precede longer sleep stretches at night. The key for breastfed babies is to maintain flexibility and respond to nursing frequency based on the baby’s cues, rather than imposing a strict schedule, particularly while milk supply is still adjusting to demand.
Formula-Fed Babies: A More Predictable Journey to 4 Hours
For formula-fed babies, the path to longer feeding intervals can sometimes appear more predictable due to the slower digestion of formula. Like breastfed infants, bottle-fed newborns should initially eat on demand, which averages about every 2 to 3 hours. Parents have the advantage of precisely measuring formula intake, which can help track consumption.
A typical bottle feeding schedule progression for formula-fed babies often looks like this:
- Newborn: Every 2 to 3 hours.
- At 2 months: Often extends to every 3 to 4 hours.
- At 4 to 6 months: Many babies can comfortably go every 4 to 5 hours.
- At 6+ months: This interval of every 4 to 5 hours often continues as solids are introduced.
It is important to ensure that the baby is consuming an appropriate feeding amount at each session. The American Academy of Pediatrics suggests a general guideline for bottle-fed babies:
| Age | Ounces per feeding | Solid foods |
|---|---|---|
| Up to 2 weeks of life | 0.5 oz. in the first days, then 1–3 oz. | No |
| 2 weeks to 2 months | 2–4 oz. | No |
| 2–4 months | 4-6 oz. | No |
| 4–6 months | 4–8 oz. | Possibly, if your baby can hold their head up and is at least 13 pounds. But you don’t need to introduce solid foods yet. |
| 6–12 months | 8 oz. | Yes. Start with soft foods, like one-grain cereals and pureed vegetables, meats, and fruits, progressing to mashed and well-chopped finger foods. Give your baby one new food at a time. Continue supplementing with breast or formula feedings. |
These are averages, and individual babies may vary. The most important aspect is to recognize your baby’s hunger and fullness cues to prevent both underfeeding and overfeeding baby, particularly since formula-fed infants can sometimes use the bottle for comfort, leading to excessive intake.
Key Signs Your Baby is Ready for a 4-Hour Feeding Schedule
Deciding when can babies go 4 hours between feedings is less about a strict age and more about observing a combination of readiness signs. These indicators suggest your baby’s digestive system has matured, their stomach capacity has increased, and they are developmentally capable of longer intervals. Rushing this transition before your baby is truly ready can lead to frustration for both parent and child.
Here are the key signs to look for:
- Baby is Sleeping Through the Night (STTN): A strong indicator of readiness is when your baby consistently sleeps for longer stretches at night, ideally 8-12 hours, without needing a feeding. The Babywise method often suggests 9-10 hours of overnight sleep before considering a 3.5-hour schedule, and longer for a 4-hour one. This shows they are consuming enough calories during the day to sustain them overnight.
- Baby Can Take Fewer Feedings: Before moving to a 4-hour schedule, your baby will likely be taking 5-6 feedings per day between typical waking hours (e.g., 7 AM to 7 PM). A true 4-hour schedule typically implies only 4 daytime feedings, potentially a fifth if a dreamfeed is still in place. Ensure your baby is physically ready to drop a feeding without compromising caloric intake.
- Baby is Always Sleeping When It is Time to Eat at 3 Hours: This is often the most significant and consistent sign. If you find yourself routinely waking your baby for their 3 or 3.5-hour feeding, and they are still deeply asleep, it’s a strong signal they are ready for a longer stretch. This indicates their nap duration is naturally extending.
- Baby Is Not Hungry at Feeding Times: When your baby shows disinterest or isn’t very hungry for meals at the current 3 or 3.5-hour intervals, they might be ready for a longer feeding schedule. They may take less milk or be easily distracted, suggesting their stomach isn’t empty yet.

- Baby Can Handle Longer Waketime Lengths: To accommodate a 4-hour feeding schedule, your baby needs to be able to stay awake for longer periods between naps. This might mean being awake for 2 hours and then sleeping for 2 hours, or being awake for 1.5 hours and then napping for 2.5 hours. Their waketime lengths need to naturally extend to fit the new rhythm.
- Baby is at Least 12 Weeks Old (Adjusted Age): While not a hard and fast rule, most babies are at least 12 weeks old before they are physiologically ready to comfortably stretch to 4-hour feeding intervals, especially when considering the reduction in total daily feedings this entails.
- Trust Your Gut: As a parent, your parental gut feeling is a powerful tool. If you strongly feel your baby is ready, it’s often worth trying a gentle transition. You can always revert to the previous schedule if it doesn’t work out.
Moving to a 4-hour schedule is a significant baby sleep patterns adjustment, impacting both feeding and sleep. It’s a developmental progression, not a race.
Transitioning to a 4-Hour Schedule: Practical Steps
Once you’ve observed the signs that your baby is ready for a 4-hour feeding schedule, the next step is a gentle and gradual feeding transition. Rushing this process can lead to an overtired or overly hungry baby, making the adjustment more challenging. The goal is to slowly lengthen the intervals between feedings while maintaining adequate intake and sleep.
- Gradual Extension: Do not jump directly from 3 hours to 4 hours. Instead, aim to add 15-30 minutes to your current feeding interval. For example, if you’re on a 3-hour schedule, try for 3 hours and 15 minutes, then 3 hours and 30 minutes, and so on. This allows your baby’s body to slowly adjust to the longer stretch without undue stress.
- Adjusting Wake Windows and Nap Lengths: A 4-hour schedule means your baby will need to either stay awake for longer periods or take longer naps. If you extend waketime, observe for signs of overtiredness. If extending naps, ensure your baby is not being woken prematurely. Some babies naturally extend their naps, others will be able to handle longer wake periods. Experiment to find what works best for your child, aiming for a balance that supports both feeding and sleep.
- Consider a Combination Schedule: It’s perfectly acceptable for your baby to have a combination feeding schedule. For instance, they might be able to go 4 hours between the first two feedings of the day but still need a 3-hour interval for later feedings. This flexibility allows you to adapt to your baby’s varying needs throughout the day.
- Observe Baby’s Cues Diligently: Throughout this transition, continuously monitor your baby for signs of hunger or discomfort. If they are fussing excessively, showing strong hunger cues well before the intended feeding time, or their naps become shorter and more restless, it may be a sign they are not ready for the extended interval.
- When to Revert: If after a few days of trying the 4-hour schedule, your baby is consistently discontent, acting hungry, or experiencing disruptions in night sleep or naps, it’s okay to adjusting routine and go back to the 3 or 3.5-hour schedule. This is not a failure; it simply means your baby needs a bit more time to develop. Patience is crucial, as this is a developmental change that cannot be forced.
Many parents find that a well-implemented sleep/feed schedule benefits the whole family, allowing for more predictable days and potentially longer stretches of night sleep. However, the child’s readiness and comfort should always be the priority.
Important Feeding Guidelines for Babies (Under 1 Year)
Beyond the schedule, what babies consume is equally vital for their healthy development. Adhering to specific infant nutrition guidelines ensures they receive the necessary nutrients while avoiding potential hazards.
- No Liquids Other Than Formula or Breast Milk: For babies under one year old, breast milk or formula should be their primary source of hydration and nutrition. Do not offer juice, cow’s milk, or other beverages. These can be upsetting to a baby’s tummy, lack the correct nutrients, and may fill them up, displacing more vital breast milk or formula intake. Water can generally be introduced in a cup around 6 months of age, when solid foods begin.

- Avoid Baby Cereal in a Bottle: This practice is generally discouraged for several reasons. It can be a choking hazard if the cereal makes the liquid too thick. A baby’s digestive system is not mature enough to properly handle cereal until around 4 to 6 months of age. Furthermore, adding cereal to a bottle can lead to overfeeding, as it may encourage excessive calorie intake without addressing true hunger.
- No Honey Until After First Birthday: Honey poses a significant risk for infants under 12 months due to the potential presence of Clostridium botulinum spores, which can cause infant botulism, a rare but serious paralytic illness.
- Adjust for Unique Needs: Every baby is unique, and some may have special feeding needs. Premature babies, for example, often follow feeding patterns based on their adjusted age. Infants with challenges such as reflux or “failure to thrive” may require a specialized feeding schedule and amount determined in consultation with their doctor. Always work with your pediatrician advice if your baby has health concerns that impact their feeding.
These guidelines ensure optimal growth and minimize risks during this critical stage of development.
Introducing Solids: How it Impacts Feeding Schedules
The introduction of solid foods, also known as complementary feeding, is an exciting milestone that typically begins between 4 and 6 months of age. This transition can significantly influence a baby’s feeding schedule, gradually leading to fewer milk feeds as solids provide more nutritional content.
Readiness Signs for Solids: Before offering solid foods, ensure your baby displays these baby solids readiness indicators:
- Good Head Control: Your baby should be able to hold their head up steadily and sit with support.
- Interest in Food: They show curiosity about what you are eating and may reach for your food.
- Opening Mouth for Spoon: They open their mouth when a spoon approaches.
- Weight: Many babies are around 13 pounds or more.
- Loss of Tongue-Thrust Reflex: The reflex that causes babies to push food out of their mouth with their tongue should have diminished.
Starting Solids: The American Academy of Pediatrics (AAP) now states that the order in which you introduce foods is less critical than previously thought. However, a key rule for complementary feeding is to introduce one new food at a time, waiting 3 to 5 days before offering another. This practice helps identify potential allergic reactions (common signs include rash, diarrhea, or vomiting). Start with soft, single-grain cereals, pureed vegetables, meats, and fruits, gradually progressing to mashed and well-chopped finger foods around 8 to 10 months.
Foods to Avoid (Choking Hazards): Be extremely cautious about choking risks. Do not offer:
- Hard foods like popcorn or whole nuts.
- Hard, fresh fruits (e.g., raw apples); cook to soften or chop into very small pieces.
- Any meat that isn’t well cooked and very finely chopped (this includes hot dogs).
- Cheese cubes.
- Whole grapes or cherry tomatoes (cut into quarters).
- Large chunks of meat or poultry.
- Honey (as mentioned, due to infant botulism risk).
- Some sticky foods like large dollops of peanut butter (discuss introducing diluted peanut butter with your pediatrician before age 1, as early introduction might prevent allergies).
As your baby approaches their first birthday, they should be eating a variety of table foods and consuming about 4 ounces of solids at each meal. Continue to offer breast milk or formula, as these remain crucial sources of nutrition. By 8 months, babies are typically still drinking about 30 ounces of milk/formula per day in addition to solids. The balance between milk feeds and solids will continue to shift as your baby consumes more food, naturally influencing their feeding intervals.
Addressing Common Challenges: Colic, Overtiredness, and Cluster Feeding
Parenting an infant comes with a unique set of challenges, many of which are intertwined with feeding and sleep. Understanding these common scenarios can help parents navigate the early months more confidently, especially when trying to establish a feeding rhythm.
Infant Colic and Feeding Frequency
Infant colic symptoms are often a source of significant parental distress. Medically defined as unexplained bouts of crying in a healthy baby, lasting at least 3 hours a day for more than 3 days a week, colic typically resolves by 3 to 4 months of age. While the exact cause is unknown, some theories link it to an immature nervous system or digestive issues. Overfeeding can exacerbate colic, highlighting the importance of mindful feeding intervals. Ensuring at least 2 to 2.5 hours pass between feeds can help prevent a baby’s digestive system from becoming overwhelmed. Managing colic often involves soothing techniques like offering a pacifier, maintaining optimal room temperature and humidity, and for breastfed babies, a review of the mother’s diet. It is crucial to consult a doctor to rule out other medical causes of intense baby crying if it persists beyond 4 months.
Cluster Feeding
Cluster feeding refers to periods when a baby feeds much more frequently than usual, often several times within a few hours. This is common in breastfed babies, particularly during growth spurts (around 3 weeks, 3 months, 6 months) or in the late afternoon/evening. It’s often misunderstood as the baby not getting enough milk, but it’s a natural behavior that helps build milk supply and can sometimes lead to longer stretches of sleep at night. While it might seem chaotic, it’s a normal and beneficial aspect of infant feeding.
Overfeeding and Weight Gain Concerns
While it’s difficult to overfeed an exclusively breastfed baby who regulates their intake, it is possible with bottle-fed infants. Babies may comfort feeding from a bottle even when not truly hungry. Signs of overfeeding can include frequent spitting up, fussiness, or excessive weight gain. Monitoring baby’s weight gain is crucial. A 2012 study showed that bottle-fed babies (regardless of milk type) gained more weight in the first year than exclusively breastfed infants. If you suspect overfeeding or have concerns about weight gain issues, your pediatrician is the best resource for guidance on appropriate feeding amounts and schedules.
Night Feedings and Sleep Disruptions
For newborns, night feedings are an absolute norm, often every 2.5-3 hours. As babies grow, they can typically go longer without feeding overnight. However, frequent night waking isn’t always about hunger. Sometimes, sleep disruptions and frequent “night snacks” can indicate accumulated fatigue from an irregular daytime schedule, an overexcited nervous system, or a negative sleep association where the baby can only fall asleep while feeding. If a child wakes every 40 minutes to an hour at night but eats well every 3-4 hours during the day, it’s unlikely to be true hunger. Observing if the baby only takes a small amount of milk before falling back asleep suggests the feed is for comfort rather than nutrition. Addressing these underlying issues, such as establishing a consistent daytime routine and promoting independent sleep, can often reduce unnecessary night feeds. It’s important to assess if the baby is receiving sufficient nutrition during the day based on weight gain before reducing night feeds.
Ultimately, understanding these common challenges allows parents to differentiate between true hunger, developmental phases, and potential issues, leading to more informed feeding decisions.
The Role of Parental Intuition and Professional Guidance
Navigating the nuances of infant feeding and the transition to a 4-hour schedule highlights the essential balance between structured advice and a parent’s innate understanding of their child. While guidelines from reputable organizations like the AAP offer invaluable frameworks, every baby is an individual with unique needs and rhythms. This is where parenting intuition becomes a powerful tool.
You, as the primary caregiver, are uniquely attuned to your baby’s subtle cues and overall disposition. If you feel your baby is ready for a change, or conversely, that a particular schedule isn’t working, trusting that instinct is paramount. Many babies naturally guide themselves toward longer feeding intervals, and sometimes, simply observing and responding to their lead can be the most peaceful approach. Forcing a schedule before a baby is developmentally ready can lead to unnecessary stress and frustration for both parent and child.
However, intuition should also be balanced with professional expertise. Your pediatrician is an invaluable resource for personalized guidance. They can assess your baby’s individualized care plan, monitor their growth and development, and help address any underlying health concerns that might impact feeding patterns. Do not hesitate to consult your pediatrician advice if you have concerns about:
- Weight gain or loss: Whether your baby is gaining too little or too much weight.
- Persistent feeding difficulties: Issues like severe reflux, difficulty latching, or constant fussiness during feeds.
- Unexplained crying or changes in behavior: Especially if these disrupt feeding or sleep significantly.
- Introducing solids: Specific advice on what foods to introduce and when, especially if there’s a family history of allergies.
Ultimately, the goal is to foster a healthy, responsive feeding relationship with your baby. This means staying flexible, understanding that phases change, and being prepared to adjust as your baby grows and develops. The path to a 4-hour feeding schedule is a journey, not a fixed destination, best traveled with a combination of informed decisions, gentle observation, and unwavering love.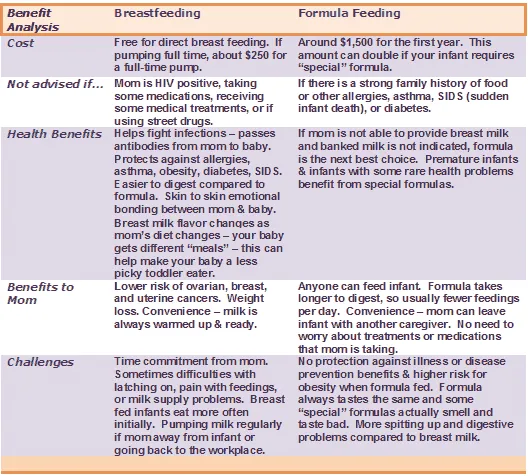
Knowing when can babies go 4 hours between feedings is a developmental milestone that brings greater predictability for families. This transition depends on a combination of factors, including the baby’s age, weight, feeding method, and individual readiness cues like sleeping through the night and showing less hunger at shorter intervals. Gradual adjustment, careful observation of the baby’s unique needs, and a balance of parental intuition with professional pediatrician advice are key to a successful transition. Remember, flexibility and patience are paramount, as every baby progresses at their own pace.


